A Great Unknown: When Flu Season and COVID Collide
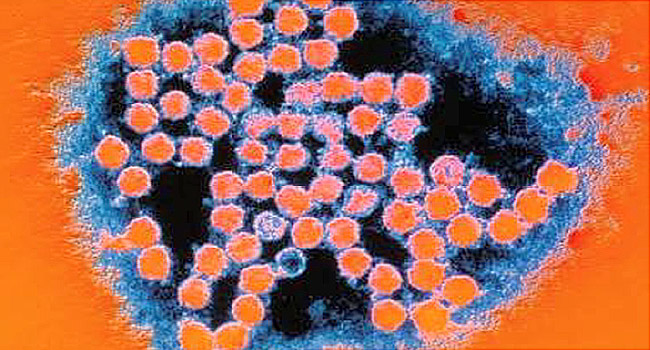
August 10, 2020 — For months scientists have urged the public to wear masks, wash their hands and socially distance. And as the flu season approaches, those practices have never been more crucial. Depending on whether people heed this advice, the U.S. could either see a record drop in flu cases or a dangerous viral storm, doctors say.
“We just have no idea what’s going to happen. Are we going to get a second surge [of coronavirus]?” says Peter Chai, MD, an emergency physician at the Brigham and Women’s Hospital in Boston. . “Hopefully, knock on wood, that won’t happen.”
To get an idea of how the flu season might go, public health officials in the U.S. often look to Australia and other countries in the southern hemisphere, where they are in the winter flu season.
This season so far in Australia, COVID-19 precautions have served to curb the pandemic while also protecting residents against the flu. Canberra had only one case for the week ending July 26, the most recent report available. It’s had 190 total cases so far this flu season – which runs March through August – compared to 2,000 last year. Activity is low in the country overall, with just 36 deaths reported so far. And that’s not just true in Australia. The World Health organization reports few cases worldwide.
But only time will tell whether the U.S. will follow suit. If not, the consequences could be dire, leaving people even more vulnerable to COVID-19 and potentially overwhelming hospitals, says Aubree Gordon, associate professor of epidemiology at the University of Michigan School of Public Health.
“There’s definitely concern about the flu overlapping with COVID. We’re hoping measures for COVID will reduce flu transmission, but that obviously isn’t guaranteed,” Gordon says. “Unfortunately, the U.S. has not done a great job of keeping COVID under wraps. This could be devastating for the health care system.”
But there are measures that could prevent that. The most important? Getting the flu vaccine as soon as possible, Gordon says.
Because flu season generally peaks between December and February, it is not yet available for most people. But when the time comes, Gordon says, the public should be especially proactive.
“People should get it as soon as it becomes available in their area,” Gordon she . “Not only to protect their health, but also for peace of mind.”
Because the flu and COVID-19 can bring similar symptoms, people who think they have COVID – but really have flu — could lead to more testing shortages as well, Gordon says.
On top of that, there is the risk of getting both at once – and having an immune system that is already compromised by the flu while contracting the coronavirus could lead to massive health emergencies, says Chai.
“Imagine getting the flu and COVID at the same time,” Chai says. “That would be terrible. There’s no reason anyone should not be getting the flu shot unless you have a true allergy to it.”
While doctors are unsure about what the next few months will bring, most can say, without hesitation, that practicing extra caution is warranted, Chai says.